Dermoscopy, also termed epiluminescence microscopy (ELM), is a noninvasive method for in-vivo evaluation of patterns of colors and microstructures of the epidermis, the dermoepidermal junction, and the papillary dermis not visible to the naked eye. There are two forms – polarized dermoscopy (PD) and non-polarized dermoscopy (NPD). NPD is generally used as contact dermoscopy with a liquid medium between the dermatoscope and the patient’s skin and has better visualization of the superficial structures in the skin (stratum corneum). PD is used as a non-contact method and provides better visualization of the deeper structures of the epidermis and dermis.
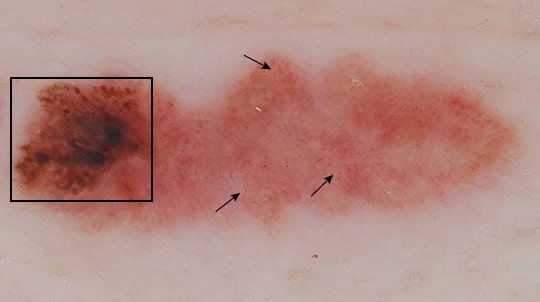
The identification of specific diagnostic patterns (pigment network, vascular structure patterns, etc) can aid the clinician in the diagnosis of malignant or benign skin lesions, thus reducing the need for biopsies. The use of this technique provides a valuable aid in diagnosing pigmented skin lesions, especially early melanoma, which may be difficult to distinguish from benign skin lesions. There are several criteria suggested to incorporate the use of dermoscopy in clinical practice (7-point checklist, three-point checklist, Menzies’ criteria, ABCD dermoscopy rule, pattern analysis, 2-step dermoscopy algorithm). Because of the complexity involved, this methodology is typically used by dermatologists — however, it has been shown to be efficacious even after brief training in the hands of non-dermatologists and primary care physicians, speaking to its wide applicability. There is evidence that dermoscopy increases diagnostic accuracy and subsequently decreases the benign to malignant ratio of biopsies needed to diagnose skin cancer (1-5).
Studies have revealed conflicting results regarding the sensitivities, specificities, and diagnostic accuracy between the different dermoscopy algorithms (6,7). These differences could be attributed to varying experience of the clinician, type of lesion examined, and small data sets (8,9). A larger data set coupled with clinicians with standardized training is required to compare the different methods in order to assess the diagnostic accuracy of the different algorithms. To that end, the ISIC project has been undertaken to establish a large bank of clinical and dermoscopy images to be followed by annotation, in order to create a centralized database that would aid in setting up international dermoscopy and total body photography standards. For more information see the International Skin Imaging Collaboration (www.isic-archive.com) or the International Dermoscopy Society (www.dermoscopy-ids.org).